Elective abdominal aortic aneurysm (AAA) repair in patients with a cancer diagnosis is associated with several poor postoperative outcomes according to a newly published study from researchers at the University of Missouri School of Medicine.
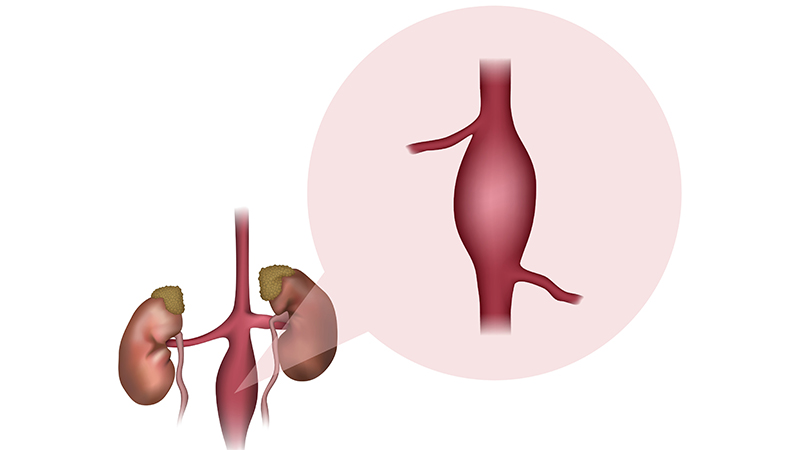
An abdominal aortic aneurysm occurs when the wall of a blood vessel weakens, causing a balloon-like dilation. A ruptured AAA is the 15th-leading cause of death in the U.S., which is why these defects are often surgically repaired when discovered. Smoking is a risk factor for both AAA and cancer.
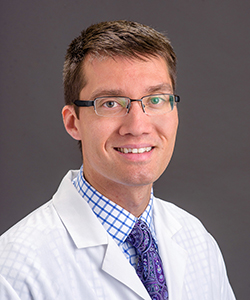
“Due to the strong association between AAA and cancer, we wanted to determine if cancer patients who underwent elective AAA repair had a greater risk of in-hospital death, cardiac complications, infection and respiratory problems compared to patients without a cancer diagnosis,” said senior author Jonathan Bath, MD, assistant professor of surgery.
Bath’s team analyzed data from the Cerner Health Facts database. Out of 8,663 patients who underwent abdominal aortic aneurysm procedures, 270 were identified with a cancer diagnosis. The researchers found patients with cancer who underwent AAA were associated with a hospital stay longer than 10 days, renal failure, respiratory problems and infection.
“We did not find that a cancer diagnosis increased the risk of in-hospital mortality, cardiac complications or stroke,” Bath said. “But cancer patients did experience more vascular complications such as bleeding, thrombosis or the need to undergo a repeat procedure.”
Researchers found male patients with a cancer diagnosis had higher odds of a prolonged length of stay, infection and respiratory failure than women with a cancer diagnosis, but there were far fewer women in the sample, making this finding less robust.
“Cancer diagnosis had no effect on mortality at 30 and 90 days unless the patient had lung cancer,” Bath said. “The mortality rate at the end of the study period was significantly higher in patients with a diagnosis of cancer than not, but many cancers will ultimately lead to patient death despite treatment. These findings illustrate the importance of careful patient selection when determining the need and type of aneurysm repair.”
Other MU School of Medicine study authors include lead investigator William Patrick Roush, MD, resident physician; Todd Vogel, MD, professor of surgery; Naveen Balasundaram, MD, assistant professor of surgery; Madelaine Behrens, medical student; Jamie Smith, research analyst; and Robin Kruse, PhD, research professor emerita.
The study, “Outcomes of Elective Abdominal Aortic Aneurysm Repair in the Setting of Malignancy,” was recently published by the Journal of Vascular Surgery. The authors declare no potential conflicts of interest.