This summer, three University of Missouri School of Medicine students began the school’s first Longitudinal Integrated Clerkship (LINC). It is a year-long intensive program that focuses on providing third-year medical students with rural health experiences. The program launched officially in June in Sedalia, Missouri, in partnership with Bothwell Regional Health Center.
In contrast to traditional block curriculum, students in the LINC program meet and follow their patients across multiple care settings and different disciplines for an entire year of medical care. This structure allows students to meet required core clinical competencies in multiple disciplines over the course of the clinical training year and encourages enduring learning relationships to develop with patients and physician-teachers.
“This is a wonderful opportunity to participate in a major advancement in medical education that has been adopted by many prestigious medical schools,” said Dr. Phil Fracica, Bothwell’s chief medical officer. “I am grateful that Bothwell has had the opportunity to ‘make history’ as the first MU training site to implement the LINC program. I believe this exciting innovation in medical education will help our students, our patients, our community and our state.”
LINC students at other universities have shown better or equivalent performance on standardized exams, clinical assessments, sub-internships and national board examinations. They also demonstrate improved measures of student patient-centeredness and empathy and greater satisfaction with clinical training than students in traditional clerkship models.
“The University of Missouri Rural Scholars program has a proven history of successfully training students in immersive rural settings,” said Laura Morris, MD, associate program director at the MU Family Medicine Residency program. “The LINC program is an innovative way to increase students’ ties to the rural community, which we know increases the odds they will return to a rural setting to practice. The continuity of care LINC students can experience will uniquely allow them to learn medicine from their patients without the limitations of short “blocks” spent in any one medical specialty.”
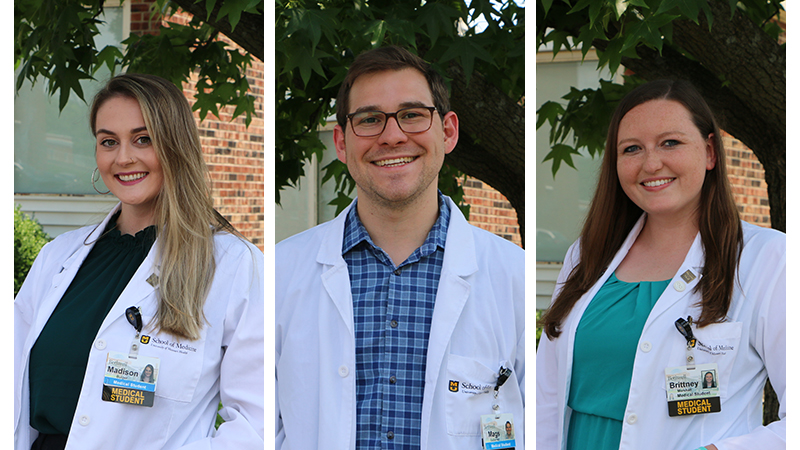
Third-year MU medical students Madison Bulger, Magdaleno Gutierrez and Brittney Marshall pursued the LINC program because they were already focusing on rural medicine in central Missouri as a part of their medical training.
“We’re learning health care in the integrated way that a patient experiences it in real life,” Marshall said. “We might see a pregnant mother at her OB/GYN visit, follow up with her in family medicine, then, when her baby's born, be a part of pediatric visits.”
The goal of rural education programs such as LINC is to inspire health care students to pursue practicing in rural areas and, long-term, to improve Missouri’s ongoing rural physician shortage.
“Before I had even started med school here at Mizzou, I knew that I wanted to focus on rural medicine, because I'm from a rural area and wanted to kind of go back to my roots,” Marshall said. “But I also want to get more hands-on experience and time with my preceptors. This program seemed like it was everything that I already loved about rural track, amplified. I feel like I’m getting a taste of practicing primary care in my third year that I might not necessarily get with the traditional curriculum.”
The program is supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) as part of an award totaling more than $7 million as of 2020.
“My dad is from a very small village of only a few hundred people in central Mexico,” Gutierrez said. “I’d go and visit as a kid and enjoyed the serenity of being in a smaller community. After having that experience then juxtaposing it with living in Los Angeles for years, I am definitely excited to not be in a huge city again. I keep falling in love with rural Missouri more and more.”





