Obstructive sleep apnea (OSA) affects an estimated 22 million Americans. In addition to sleep problems, the condition can cause other health issues, including high blood pressure, chronic heart failure and stroke.
Some patients with OSA are at an even higher risk of cardiovascular problems because of a phenomenon called “reverse dipping” that causes blood pressure to rise rather than lower during sleep. Most people experience lower blood pressure at night. Now, University of Missouri School of Medicine researchers have found a potential cause for reverse dipping that may help patients with OSA get the help they need before cardiovascular disease develops.

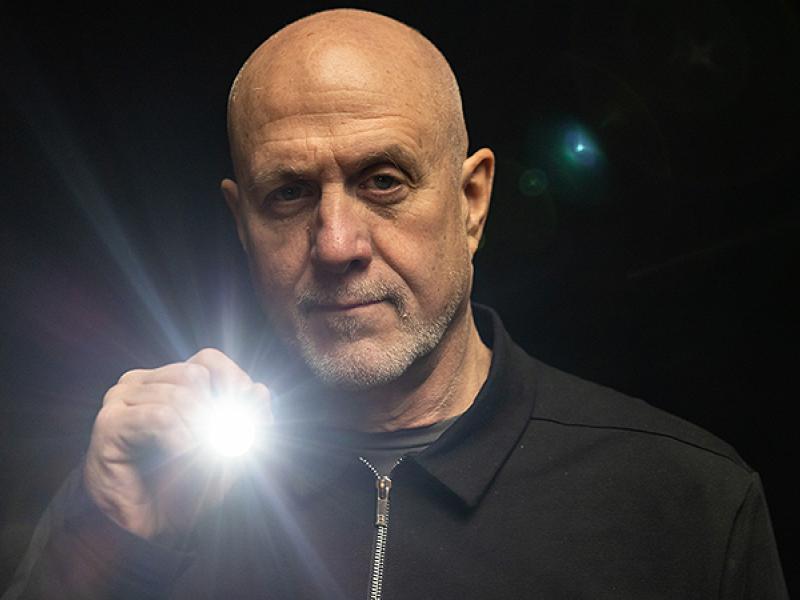
“We can now identify those with OSA at the highest risk of cardiovascular problems in order to prevent them from developing additional complications,” said David Gozal, MD, the former Marie M. and Harry L. Smith Endowed Chair of Child Health at the MU School of Medicine. “We can treat those patients more aggressively to ensure they adhere to therapy and use their continuous positive airway pressure device (CPAP) properly.”
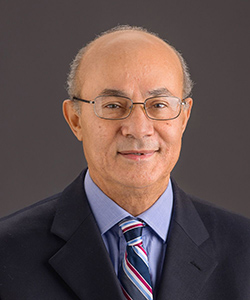
Gozal and fellow MU collaborator Abdelnaby Khalyfa, PhD, studied 46 patients diagnosed with OSA. They ranged in age from 18 to 70. Fifteen participants were identified to have a rise in blood pressure during sleep, while the remaining 31 participants had blood pressure readings that either remained the same or declined at night. The researchers collected blood from each participant to study the messages cells produce and send to each other through microscopic packages called exosomes.
“We found that the cell messages coming from participants with night-time elevated blood pressure were different than those transmitted in subjects with normal blood pressure,” Gozal said. “The altered messages caused the cells that line the blood vessels to become dysfunctional. Those disturbed vessels allowed inflammatory cells to enter the vessels’ walls, causing hardening of those vessels and leading to cardiovascular disease.”
Gozal said the cell message discovery will help clinicians personalize treatment for each patient diagnosed with OSA. A simple blood test administered at the beginning of a sleep study could indicate each patient’s cardiovascular risk.
Gozal said additional research is needed to study the patients at highest risk of cardiovascular complications from OSA to see if CPAP compliance can actually reduce blood pressure or normalize the cell messages used to determine a patient’s risk.
In addition to Gozal and Khalyfa, the study authors include Bharati Prasad, MD, University of Illinois Hospital and Health Sciences System; and Wen-Ching Chan, PhD, and Jorge Andrade, PhD, of the University of Chicago’s Center for Research Informatics.
The study, “Circulating Plasma Exosomes in Obstructive Sleep Apnea and Reverse-Dipping Blood Pressure,” was recently published in the European Respiratory Journal. Research reported in this publication was supported by the U.S. Department of Veterans Affairs. The authors of the study declare that they have no conflicts of interest related to this study. The content is solely the responsibility of the authors and does not necessarily represent the views of the funding agencies.