The National Institutes of Health (NIH) has awarded University of Missouri School of Medicine researchers a grant to test a technique to provide Type 1 diabetes patients with insulin-producing beta cells that don’t come from another person’s pancreas — a potentially life-changing treatment for millions who require several insulin injections daily.

Pancreatic islet transplantation is an experimental treatment for Type 1 diabetes in which surgeons transplant clusters of pancreas cells from a deceased donor into a vein that carries blood to the liver of a person with Type 1 diabetes. The cell clusters then make and release insulin in the recipient’s body, potentially preventing the need for regular insulin injections. A major limitation of islet transplantation is the scarcity of donors and the need for lifelong use of immunosuppressive drugs to control rejection.
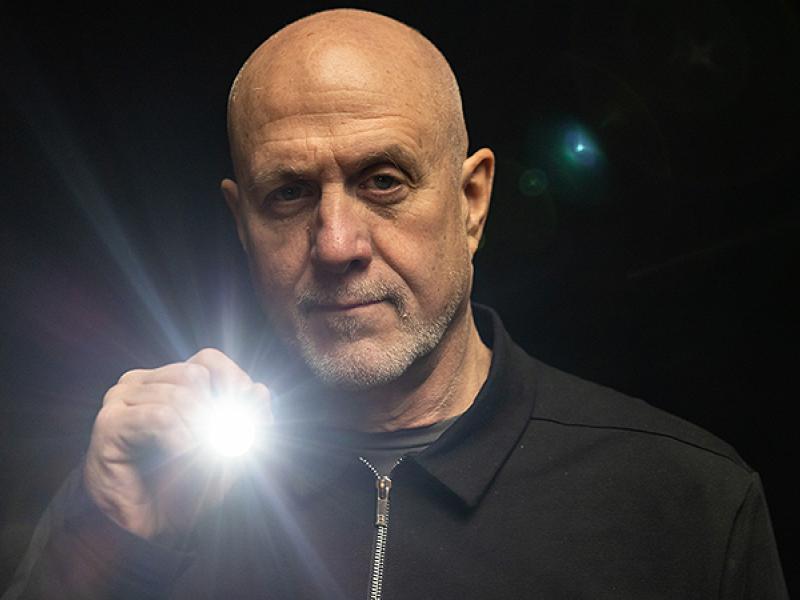
MU School of Medicine researchers Haval Shirwan, PhD, and Esma Yolcu, PhD, both professors of Child Health and Molecular Microbiology and Immunology, are part of a grant with Andrés García, PhD, executive director, Parker H. Petit Institute for Bioengineering and Bioscience at the Georgia Institute of Technology, to study a novel approach where a type of self-renewing stem cell is converted into an insulin-producing beta cell, then clusters of those cells are transplanted from a test tube into patients with Type 1 diabetes. To protect the stem cells from rejection, the transplant will include a microgel mixture that contains a protein designed to kill only the T-cells that identify the transplanted cells as a foreign threat.

“There is an unlimited source of stem cells, which solves the bottleneck currently associated with donor cells,” Shirwan said. “Dr. García and team will generate these cells that will be mixed with microgels engineered with a protein we generated, the microgel will stay with the transplanted cells, and when the immune system’s T-cells come to attack, the protein will eliminate them, without disrupting other immune cells.”
The stem cell to beta cell conversion transplant will initially be tested on mice. If successful, it would eventually be tested on humans, with the potential to benefit those suffering from similar chronic diseases.
“The potential is huge if this technique is successful,” Yolcu said. “The sustained survival and function of these cells without continuous use of immunosuppression will widen their use for other indications, such as Type 2 diabetics.”
Shirwan and Yolcu are among the first researchers working in the newly opened Roy Blunt NextGen Precision Health building at the University of Missouri. This initiative is designed to expand collaboration in personalized health care and the translation of interdisciplinary research for the benefit of society. The NextGen Precision Health building at Mizzou anchors this statewide initiative, which aims to unite government and industry leaders with innovators from across the system’s four research universities in pursuit of life-changing precision health advancements. The University of Missouri System’s bold NextGen initiative highlights the promise of personalized health care and the impact of large-scale interdisciplinary collaboration.
The NIH grant is worth nearly $2 million over five years.