By age 75, approximately half of all Americans will develop cloudy vision caused by cataracts, according to the National Eye Institute. The most common complication from cataract surgery is high eye pressure, which can cause swelling and other issues that can lead to vision loss or even blindness. Now, researchers from the University of Missouri School of Medicine recommend a new test to check eye pressure to prevent possible vision loss.
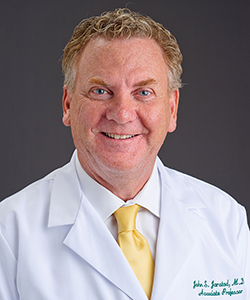
“The current standard of care following cataract surgery is to refill the eye with a saline solution and tap on the eye with a Q-tip to observe if it is too firm, too soft or just right,” said John Jarstad, MD, associate professor of ophthalmology at the MU School of Medicine and lead researcher of the study. “This Goldilocks-style guesstimate often is inaccurate, and patients might actually have higher eye fluid pressure than the surgeon believes. Here at MU Health Care, we use a device known as a tonometer to accurately gauge eye pressure.”
An electronic eye pressure monitoring device known as a tonometer often is used in a clinical setting to determine eye pressure, but the device rarely is used in a surgical setting. The researchers studied 170 patients who had eye pressure adjusted after cataract surgery with a tonometer and found that patients were 2.5 to 4 times less likely to develop cystoid macular edema — cyst-like pockets of fluid in the macula of the eye.
According to Jarstad, normal eye pressure should be between 16 and 21 mmHg, or millimeters of mercury. In most cases, a high eye pressure will resolve itself in a matter of days without issue, but in cases in which the pressure is significantly high, a person can experience symptoms of nausea and pain above the eyebrow. In these cases, it’s important that the pressure be adjusted to prevent permanent damage to the eye.
A tonometer costs eye surgeons approximately $4,000, though its use can save patients up to $150 in medications and eye drops used to treat retinal swelling or edema. A lower cost pressure ring also can be used as an effective alternative tool to gauge eye pressure, Jarstad said. Potential complications from using a pressure monitoring device include eye infections, though Jarstad has not observed an infection in five years of using a pressure monitor.
“Seeing patients who had gone blind because of high eye pressure convinced me that there needed to be a better, more accurate gauge,” Jarstad said. “I recommend eye surgeons adopt this practice for the good of their patients. There is no additional cost to patients, and if it saves just one patient from going blind, it would be well worth every doctor using it in his or her surgical practice.”
The study, “Immediate IOP Adjustment in Operating Theater — Is there any Benefit?” recently was presented at the annual meeting of the Indonesian Ophthalmologists Association. Research reported in this publication was supported by the MU Department of Ophthalmology. The researchers have no conflicts of interest to declare related to this study.