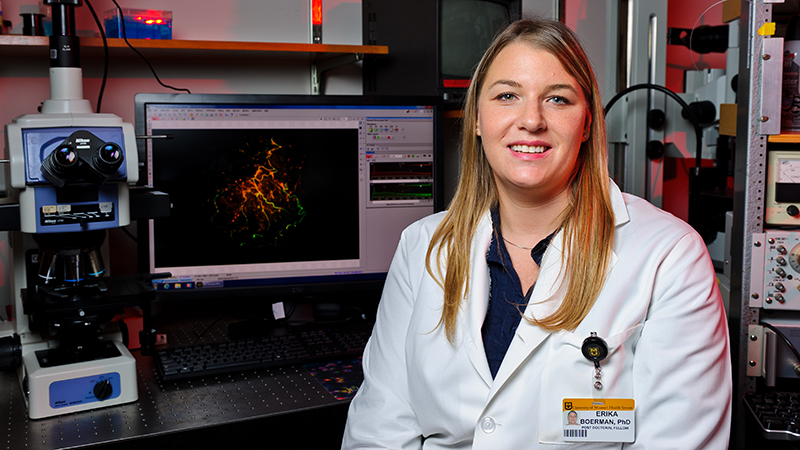
The National Institutes of Health (NIH) has awarded Erika Boerman, PhD, an assistant professor at the University of Missouri School of Medicine, a $1.8 million grant to study the role a specific set of perivascular nerves play in the development of inflammatory bowel disease (IBD).
IBD includes two major chronic conditions, Crohn’s disease and ulcerative colitis, that cause inflammation in the intestinal tract when the immune system responds to an environmental, genetic, or microbial trigger. IBD is rising dramatically in the U.S. and across the globe. There is no cure.
Boerman’s research will test the hypothesis that neurotransmitters released from perivascular sensory nerves (PSN) on the mesenteric arteries — which distribute blood from the abdominal aorta to a large portion of the gastrointestinal tract — trigger immune cell activation and inflammation that restricts blood flow to the intestines, a hallmark symptom of IBD.
“Very few studies to date have addressed vascular dysfunction with IBD, especially in the context of immune cell infiltration,” Boerman said. “A lack of blood flow to the gut is a major problem associated with IBD. Any new avenue we can explore to improve quality of life for those with IBD is important.”
Boerman will investigate the IBD development process in mice to determine how it negatively affects blood flow to the gut.
“We want to know over the course of the development of the disease if immune cell infiltration into the blood vessel wall happens first, or if you get impaired sensory nerve function, decreased blood flow then an influx of immune cells,” Boerman said. “We want to know the order of events that leads up to this accumulation of immune cells and decrease in perivascular nerve function that ultimately causes the blood vessels to dilate.”
Another aim of the grant is to identify whether immune cells are intercepting perivascular nerve transmitters designed to instruct blood vessel cells to relax and allow more blood flow. Boerman believes the immune cells are hijacking those molecules and then accumulating in the cell wall, hindering blood flow instead of helping it. Understanding that dynamic could help identify a potential treatment to prevent the immune cell accumulation, which would reverse inflammation, restore blood flow and alleviate IBD symptoms.
“We have some good treatment strategies for Crohn’s disease and ulcerative colitis, but there’s a need to develop better medications to manage those symptoms,” Boerman said. “Our goal is to provide new insights toward developing selective therapeutic strategies for treating blood vessel dysfunction and impaired blood flow to the intestines in hopes of improving quality of life for IBD patients.”
The NIH grant is a five-year, $1.85 million award that runs through May 2026.