An electronic health record (EHR) program to help primary care doctors address child obesity is an effective tool to promote positive body mass index (BMI) trends, especially among young children with obesity, according to a new University of Missouri School of Medicine study that examined the effectiveness of the FitTastic tool over an average follow-up period of nearly three years.
FitTastic was developed in 2011 to support health care teams in communicating with families about five lifestyle behaviors: aiming for at least one hour per day of physical activity, limiting screen time to two hours per day or less, drinking three servings a day of low-fat milk or calcium, drinking at least four servings per day of water instead of sugary drinks and eating at least five servings per day of fruits and vegetables.
The FitTastic intervention includes a patient behavior assessment, an EHR interface that supports providers with the behavior data for use in goal setting with the family, discussion of the FitTastic goals, and a handout and participation incentives to encourage families to achieve the goal such as a frisbee or water bottle.
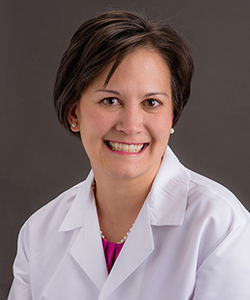
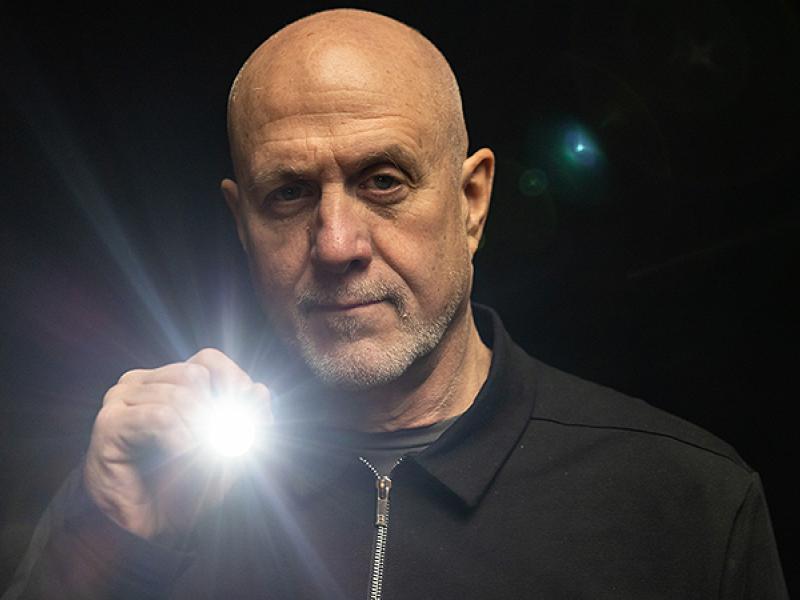
“Childhood obesity is a growing problem in Missouri and across the country which has been exacerbated by the COVID 19 pandemic,” said principal investigator Amy Braddock, MD, associate professor of clinical family and community medicine. “Over 30% of children in this country meet criteria for obesity or being overweight. Primary care providers have an opportunity to play a pivotal role in providing screening and counseling for obesity, and we wanted to test the long-term effectiveness of FitTastic as a tool to help in this effort.”
Braddock’s team conducted a multi-year study to determine if overweight or obese children at the beginning of the study exhibited a more favorable body mass index (BMI) trajectory in clinics that used the FitTastic tool over a period of years, compared to children seen at clinics without the tool.
“We found a nearly 20% more favorable BMI pattern in the FitTastic group compared to the control group when looking specifically at children who were either overweight or obese,” Braddock said. “The data was especially favorable for younger children, between the ages of two and five-years-old.”
Braddock’s team discovered parental educational level was a risk factor for child obesity at the beginning of the study, but the results showed no influence of parental education on the BMI pattern of FitTastic versus control participants, suggesting that FitTastic can be equally effective in children with parents of different educational levels.
“The marriage of clinic-based interventions and EHR data assessment offers the opportunity for significant innovation and can be useful for partnering health care teams and families in the important tasks of setting positive, family-centered healthy lifestyle goals,” Braddock said. “FitTastic is the first of hopefully many new and exciting technologies to support physicians working with families to promote positive health behaviors. Only by developing creative new approaches that improve the environments that our children live in can we expect to curb the child obesity epidemic.”
Braddock’s MU co-authors included Richelle Koopman, MD, the Jack M. and Winifred S. Colwill Endowered Professorship in Family and Community Medicine; Jamie Smith, research analyst; medical students Andy Lee and Natalie Miller; Samuel Holt McNair, MD, resident physicians; Nuha Wareg, research specialist; and Megan Clary, MD, assistant professor of clinical child health.
“A Longitudinal Effectiveness Study of a Child Obesity Electronic Health Record Tool,” was recently published by the Journal of the American Board of Family Medicine. Funding was provided by the American Academy of Family Physicians Foundation Joint Grant Award Program. The findings and conclusions in this article are those of the authors and do not necessarily represent the official positions of the American Academy of Family Physicians.
The authors declare no conflicts of interest.