Glioblastoma is an aggressive and deadly brain cancer. Although improved treatment protocols have doubled the survival rate over the past 20 years, glioblastoma tumors usually grow back. After surgeons remove the tumor, patients typically undergo surveillance imaging within 48 hours followed by regular screenings to monitor for recurrence. However, a retrospective study from the University of Missouri School of Medicine and MU Health Care showed patients who underwent surveillance imaging after surgery did not have better outcomes than patients who did not have imaging and returned when they felt symptoms of recurrence.

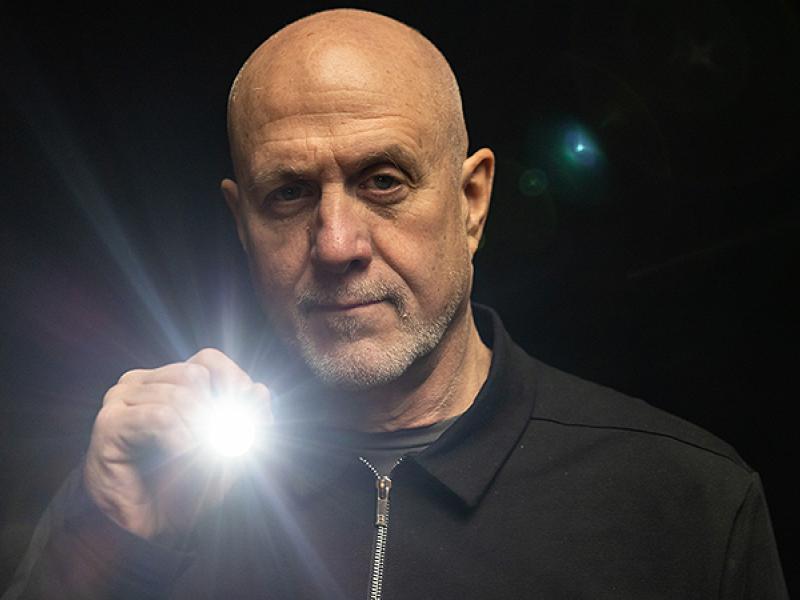
“Patients who undergo regular imaging can become nervous or anxious in the days or weeks leading up to their imaging appointment,” said N. Scott Litofsky, MD, professor and chief of neurological surgery at the MU School of Medicine and MU Health Care. “While surveillance is good, maybe we can change our protocols to make patients more comfortable and give them more control of the process but still deliver quality care.”
Litofsky’s research team reviewed 74 cases at MU Health Care. Of those, 47 patients underwent routine surveillance and 27 returned when they felt symptoms of recurrence. Litofsky found the median survival without a worsening condition was 6.1 months for the surveillance group and 6.0 for the symptomatic group. Post-recurrence survival rates were 6.4 months for surveillance and 7.7 months for symptomatic cases.
“We have a lot of patients who come from a long distance, and our general philosophy of care is to provide regular follow-up visits,” Litofsky said. “The hypothesis was patients would do better if we did regular surveillance. The results indicated that for this population of patients, the outcome was equivalent whether they had surveillance or showed up when they had symptoms.”
Litofsky said less patient surveillance testing could improve patient convenience, reduce cost and ease pre-imaging anxiety.
“Sometimes we do things because they seem to be the right thing to do, even if the evidence suggests maybe we don’t need to do it,” Litofsky said. “We may need to change our paradigm on how we are taking care of these patients.”
Litofsky is now planning a pilot study to link patient-reported outcomes identified through a questionnaire to clinic visits for patients. Then he’ll examine if the patient-reported outcomes are superior to clinic visits that included surveillance imaging.
“Maybe down the road, we could use a combination of reported outcomes and surveillance so we can reduce the amount of time the patients need to spend coming to appointments,” he said.
Litofsky’s study, “Does Surveillance-Detected Disease Progression Yield Superior Patient Outcomes in High-Grade Glioma?” was recently published by the journal World Neurosurgery. Research reported in this publication was supported by the University of Missouri Research Council Summer Research Fellowship and Head for the Cure Foundation philanthropic gift. The authors of the study declare that they have no conflicts of interest. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies.