According to the World Health Organization, approximately 37 million people are living with HIV. Antiviral medications are used to control the disease and prevent its progression to AIDS. Although antivirals improve health and increase survival for people with HIV, their use also has been linked to the development of cardiovascular disease.
Now, researchers at the University of Missouri School of Medicine have identified an enzyme that may reduce the risk of cardiovascular disease caused by HIV medications.
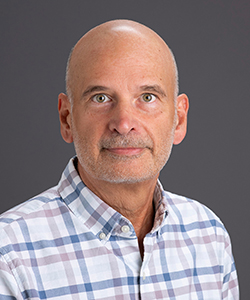
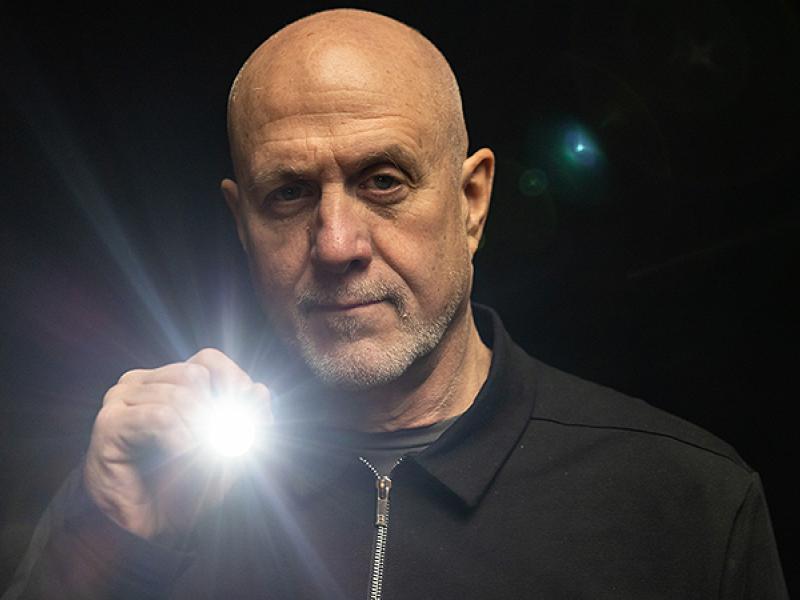
“The use of antivirals in HIV patients is very important to control the virus, suppress symptoms and improve quality of life,” said William Durante, PhD, a professor of medical pharmacology and physiology at the MU School of Medicine and lead author of the study. “However, antivirals also are linked to the development of metabolic disorders such as diabetes and obesity, and they are known to increase the risk of cardiovascular disease. Our study focused on protease inhibitors, a very common antiviral used to treat HIV.”
Protease inhibitors disrupt HIV’s ability to replicate and infect cells. However, they also cause endothelial cell malfunction, which can lead to cardiovascular disease.
“Endothelial cells make up the inner lining of blood vessels and are essential to vascular health,” Durante said. “When protease inhibitors are used to treat HIV, endothelial cell function is compromised. The cells’ natural tendency to promote blood flow through the vessel is lost and they also become inflamed. These issues lead to plaque build-up within arteries and, ultimately, cardiovascular disease.”
Durante and his research team knew from previous studies that the enzyme heme oxygenase-1, or HO-1, offers protection against endothelial dysfunction. Using a cell-based model of cultured human endothelial cells, the researchers were able to increase the amount of the enzyme within the cells.
“Increasing the presence of HO-1 in our model before exposing it to a protease inhibitor allowed the medication to do its job without causing endothelial dysfunction,” Durante said. “HO-1 shows great promise as a defender of endothelial cells in patients being treated for HIV.”
More research is needed to verify that HO-1 will prevent endothelial cell dysfunction with all antiviral medications. However, Durante feels that identifying the enzyme’s role in reducing vascular inflammation with protease inhibitors may one day make it a new option for preventing cardiovascular disease caused by HIV medications.
The study, “Heme Oxygenase-1-Derived Bilirubin Counteracts HIV Protease Inhibitor-Mediated Endothelial Cell Dysfunction,” recently was published in Free Radical Biology and Medicine. Funding for the study was provided by the National Heart, Lung and Blood Institute of the National Institutes of Health (R01HL59976). The content of the article is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies.