The gene editing technique known as CRISPR is a revolutionary approach to treating inherited diseases. However, the tool has yet to be used to effectively treat long-term, chronic conditions.
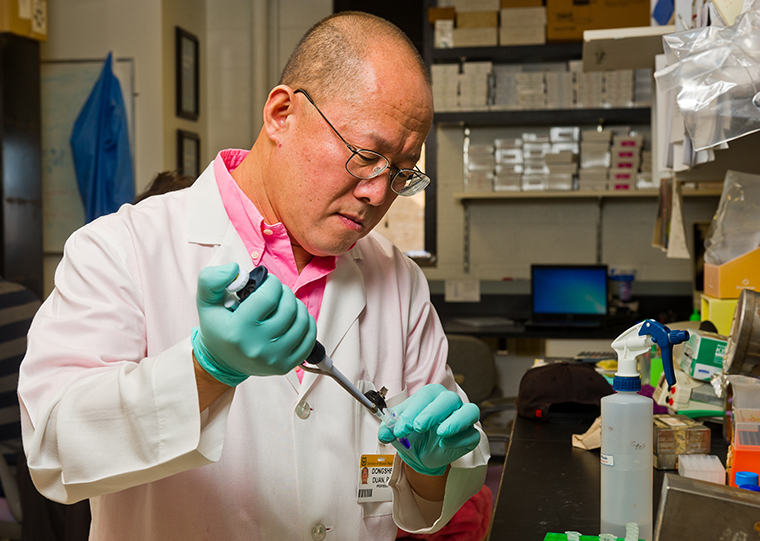
A research team led by Dongsheng Duan, PhD, at the University of Missouri School of Medicine has identified and overcome a barrier in CRISPR gene editing that may lay the foundation for sustained treatments using the technique.
CRISPR gene editing is inspired by the body’s natural defensive ability to fend off viruses. The technology enables researchers to alter DNA sequences by cutting out and replacing a mutation in the genome, which has the potential to treat a variety of genetic diseases and conditions. Duan, along with his collaborators at MU, the National Center for Advancing Translational Sciences at the National Institutes of Health and Duke University, are studying how to harness CRISPR to treat Duchenne muscular dystrophy (DMD).
Children with DMD have a gene mutation that interrupts the production of a protein known as dystrophin. Without dystrophin, muscle cells become weaker and eventually die. Many children lose the ability to walk, and muscles essential for breathing and heart function ultimately stop working.
“CRISPR essentially cuts out the mutation and stitches the gene back together,” said Duan, who serves as the Margaret Proctor Mulligan Professor in medical research in the Department of Molecular Microbiology and Immunology at the MU School of Medicine. “In order to do this, the ‘molecular scissors’ in CRISPR, known as Cas9, must know where to cut. The location to cut is flagged by a molecule called gRNA. We were surprised to find that by increasing the quantity of flags, we could extend the effectiveness of the therapy from three months to 18 months in our mouse model.”
Duan’s lab treated 6-week-old mice with DMD intravenously using CRISPR and looked for improvements at 18 months. They initially employed a strategy widely used by many researchers. In this approach, similar amounts of Cas9 and gRNA were administrated. While it worked well when injected directly into the muscle, this strategy yielded poor outcomes when the team tried to achieve long-term correction in all the muscles in the body. They found no dystrophin restoration in skeletal muscle and low-level dystrophin restoration in the heart — the treatment failed to stop disease progression.
When reviewing the results, the team found a disproportionate depletion of gRNA flags, meaning there were not enough gRNA to tell Cas9 where to cut. The team increased the number of gRNA flags and repeated the experiment. This new strategy significantly increased dystrophin restoration in both heart and skeletal muscle and reduced muscle scarring at 18 months. Additionally, muscle function and cardiac function were improved.
“Our results suggest that gRNA loss is a unique barrier for long-term systemic CRISPR therapy,” Duan said. “We believe this barrier can be overcome by increasing and optimizing gRNA doses. While this has exciting possibilities for improvements to DMD therapies, we believe this principle may also be applied to other CRISPR therapies for a range of other diseases and conditions.”
The researchers will continue to test and refine the approach in a mouse model before other models are explored. With more study, they are hopeful this insight may help lay the foundation for improved therapies using CRISPR gene editing.
The study, “AAV CRISPR Editing Rescues Cardiac and Muscle Function for 18 Months in Dystrophic Mice,” was recently published online by JCI Insight. Authors include Duan lab members Nalinda Wasala, Lakmini Wasala, Yongping Yue, Jacqueline Louderman, Thais Lessa, Aihua Dai, Keqing Zhang, Gregory Jenkins, Michael Nance, Xiufang Pan and Kasun Kodippili; collaborator Shi-jie Chen from the Department of Physics, Department of Biochemistry and the Informatics Institute at MU; collaborators Chady Hakim and Nora Yang with the National Center for Advancing Translational Sciences; and collaborators Christopher Nelson and Charles Gersbach with Duke University.
The research was funded by the National Institutes of Health (AR-69085, GM-063732 and GM-117059), the Intramural Research Program of the NIH National Center for Advancing Translational Sciences, the Department of Defense (MD15-1-0469 and MD150133), Hope for Javier, the Jackson Freel DMD Research Fund, the Muscular Dystrophy Association (MDA277360) and the Duke Coulter Translational Partnership.
Duan is a member of the scientific advisory board and equity holder of Solid Biosciences LLC. Duan and Yue are inventors on patents (unrelated to this study) that were licensed to Solid Biosciences LLC. The Duan lab has received research supports unrelated to this project from Solid Biosciences LLC. Hakim, Duan, Wasala and Yue have filed a patent application related to the findings described in this paper. Gersbach has filed patent applications related to genome editing for Duchenne muscular dystrophy. Gersbach is an adviser to and receives research support from Sarepta Therapeutics Inc. Gersbach and Nelson are inventors on patent applications related to genome editing.