It’s no secret – cardiac magnetic resonance imaging exams, or cardiac MRIs, aren’t exactly fun.
The exams are used to detect and monitor disease and evaluate the heart’s anatomy and function. However, they often require patients to spend a long time in a tight space.
Cardiac MRI exams can last 45 to 90 minutes and require multiple 10- to 20-second breath holds by the patient. The procedure can be exhausting for patients, particularly frail patients with breathing difficulties who are unable to hold their breath.
A team of researchers at the University of Missouri is working to fix that problem through a project called HeartSpeed. HeartSpeed uses data analysis software to eliminate the need for patients to hold their breath.
“We found that we could separate breathing motion from the heart motion quite well using the software, and we thought we should try to start applying this to real patient data to make a clinical tool,” said Steve Van Doren, PhD, a professor of biochemistry at MU.
The goal is a more comfortable scan in which patients are able to breathe freely. Shorter procedure times will also result in increased efficiency and lower costs.
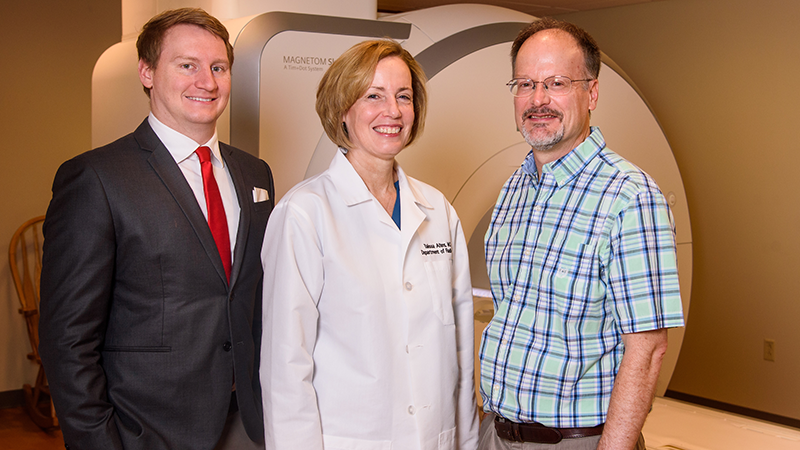
“Patients will benefit because it will be easier for them to do the exam. Hopefully, the radiologist or cardiologist who reads the MRI will benefit, because the images will be much better,” said Talissa Altes, MD, chair of the Department of Radiology at the MU School of Medicine.
Researchers believe their work will produce more information specific to the patient’s cardiac function within a single imaging session. For example, doctors would be able to spot a slight murmur or arrhythmia – conditions that conventional MRI is unable to pick up.
“The data itself that we get back, that will be specific to each individual patient and specific to their pathology in a way that we haven't been able to acquire in the past,” said Robert Thomen, PhD, an assistant professor of radiology and bioengineering.
Doctors will then be able to recommend therapies that are better catered to the individual patient – an idea known as precision medicine.
The HeartSpeed team brings together researchers and clinicians from a variety of disciplines, including medicine, engineering and biochemistry.
“Working across departments can really accelerate research efforts toward clinical translation,” Thomen said. “That’s what this whole research philosophy is about with the NextGen Precision Health Institute.”

Highlighting the promise of personalized health care and the impact of large-scale interdisciplinary collaboration, the NextGen Precision Health initiative is bringing together innovators from across the University of Missouri and the UM System’s three other research universities in pursuit of life-changing precision health advancements. It’s a collaborative effort to leverage the research strengths of Mizzou toward a better future for the health of Missourians and beyond. The Roy Blunt NextGen Precision Health building at MU anchors the overall initiative and expands collaboration between researchers, clinicians and industry partners in the state-of-the-art research facility.