Over the past two decades, the number of new diabetes cases has almost tripled in the U.S., and 80% of patients with Type 2 diabetes die from cardiovascular disease. A University of Missouri research team recently received two grants totaling more than $6 million from the National Institutes of Health to study how vascular disease develops in people with Type 2 diabetes.
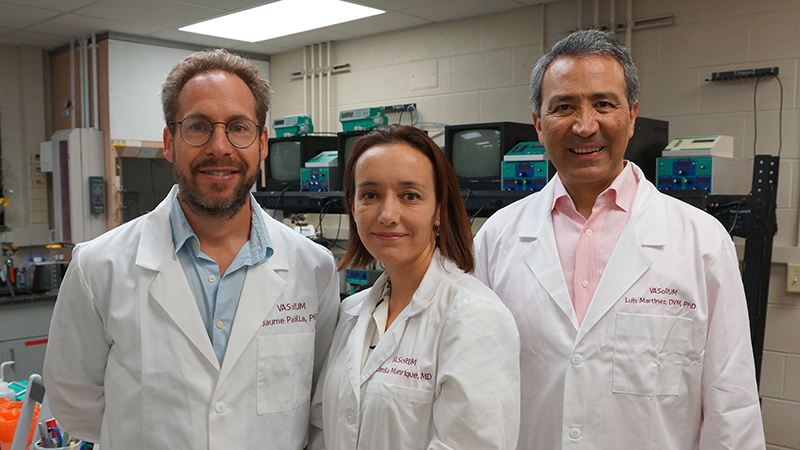
“New interventions are needed to minimize the impact of diabetes on the vascular system,” said Camila Manrique-Acevedo, MD, associate professor of medicine. “We want to explore the mechanisms behind the diabetes-triggered disruptions to the cardiovascular system and test potential treatments that could translate into better outcomes for these patients.”
One grant will test the ability of the plant-based supplement phosphatidylserine to inhibit an enzyme known as ADAM17, which disrupts normal blood vessel function.
“We’re going to improve how blood vessels respond to insulin,” said Luis Martinez-Lemus, DVM, PhD, professor of medical pharmacology and physiology. “We believe that if we can increase circulating levels of phosphatidylserine, this will neutralize the ability of ADAM17 to cause insulin resistance in the blood vessel.”
The other grant will fund research that targets the enzyme neuraminidase, which disrupts cell structures in the vessels that sense blood flow.
“In Type 2 diabetes, the blood-flow-sensing structures in the vessels are destroyed,” Martinez-Lemus said. “We propose to reduce the activity of the neuraminidase enzyme, thus reducing the degradation of these sensors and normalizing vascular function.”
“Certain anti-viral drugs inhibit neuraminidase enzymes and will be used to study their vascular benefits in diabetic mice and humans,” added Jaume Padilla, PhD, associate professor of nutrition and exercise physiology.
Manrique-Acevedo, Martinez-Lemus and Padilla are among the first wave of researchers who will move into the NextGen Precision Health building, which is scheduled to open in October. The NextGen Precision Health initiative brings together researchers from across the University of Missouri’s four campuses, along with clinicians and industry leaders in a state-of-the-art facility. The initiative aims to foster team science and shorten the nearly two-decade journey it takes for research findings to change clinical practice.
“Both of those projects have a basic science component and a clinical trial component, nicely suiting the mission of NextGen,” Padilla said. “We are excited to capitalize on the fantastic infrastructure and resources available at NexGen. We envision the move to NextGen will expand the scope of our collaborative and translational work and catapult our team toward making new discoveries to ultimately prevent and treat cardiovascular disease in diabetes.”

Highlighting the promise of personalized health care and the impact of large-scale interdisciplinary collaboration, the NextGen Precision Health initiative is bringing together innovators from across the University of Missouri and the UM System’s three other research universities in pursuit of life-changing precision health advancements. It’s a collaborative effort to leverage the research strengths of Mizzou toward a better future for the health of Missourians and beyond. The Roy Blunt NextGen Precision Health building at MU anchors the overall initiative and expands collaboration between researchers, clinicians and industry partners in the state-of-the-art research facility.