New research from the University of Missouri School of Medicine has established a link between western diets high in fat and sugar and the development of non-alcoholic fatty liver disease, the leading cause of chronic liver disease.
The research, based in the Roy Blunt NextGen Precision Health Building at MU, has identified the western diet-induced microbial and metabolic contributors to liver disease, advancing our understanding of the gut-liver axis, and in turn the development of dietary and microbial interventions for this global health threat.
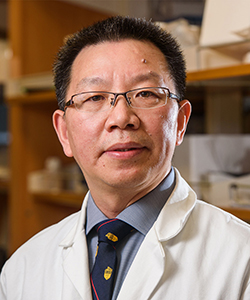
“We’re just beginning to understand how food and gut microbiota interact to produce metabolites that contribute to the development of liver disease,” said co-principal investigator, Guangfu Li, PhD, DVM, former associate professor in the department of surgery and Department of Molecular Microbiology and Immunology. “However, the specific bacteria and metabolites, as well as the underlying mechanisms were not well understood until now. This research is unlocking the how and why.”
The gut and liver have a close anatomical and functional connection via the portal vein. Unhealthy diets change the gut microbiota, resulting in the production of pathogenic factors that impact the liver. By feeding mice foods high in fat and sugar, the research team discovered that the mice developed a gut bacteria called Blautia producta and a lipid that caused liver inflammation and fibrosis. That, in turn, caused the mice to develop non-alcoholic steatohepatitis or fatty liver disease, with similar features to the human disease.
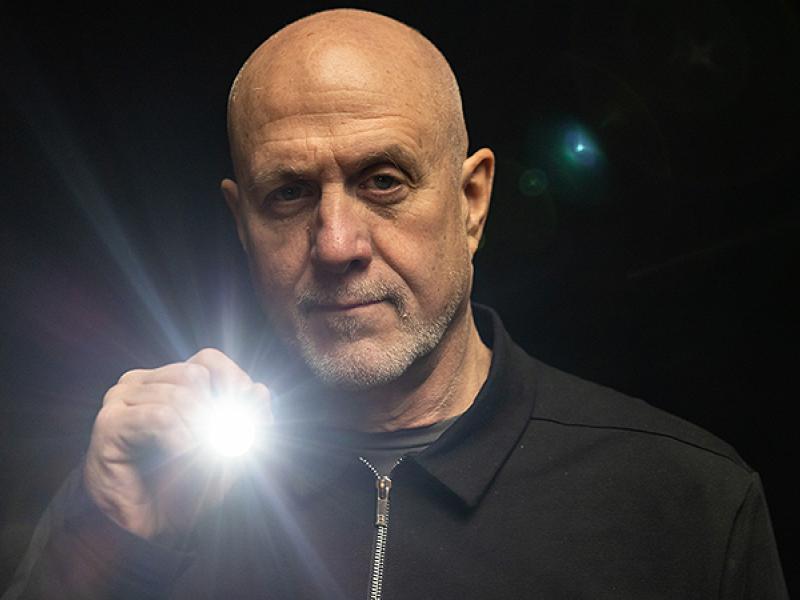
“Fatty liver disease is a global health epidemic,” said Kevin Staveley-O’Carroll, MD, PhD, former professor in the department of surgery, one of the lead researchers. “Not only is it becoming the leading cause of liver cancer and cirrhosis, but many patients I see with other cancers have fatty liver disease and don't even know it. Often, this makes it impossible for them to undergo potentially curative surgery for their other cancers.”
As part of this study, the researchers tested treating the mice with an antibiotic cocktail administered via drinking water. They found that the antibiotic treatment reduced liver inflammation and lipid accumulation, resulting in a reduction in fatty liver disease. These results suggest that antibiotic-induced changes in the gut microbiota can suppress inflammatory responses and liver fibrosis.
Li, Staveley-O'Carroll and fellow co-principal investigator R. Scott Rector, PhD, Director of NextGen Precision Health Building and Interim Senior Associate Dean for Research — are part of NextGen Precision Health, an initiative to expand collaboration in personalized health care and the translation of interdisciplinary research for the benefit of society. The team recently received a $1.2 million grant from the National Institutes of Health to fund this ongoing research into the link between gut bacteria and liver disease.
The study, “Western diet contributes to the pathogenesis of non-alcoholic steatohepatitis in male mice via remodeling gut microbiota and increasing production of 2-oleoylglycerol” was recently published in Nature Communications. The authors declare that they have no conflicts of interest related to the study.

Highlighting the promise of personalized health care and the impact of large-scale interdisciplinary collaboration, the NextGen Precision Health initiative is bringing together innovators from across the University of Missouri and the UM System’s three other research universities in pursuit of life-changing precision health advancements. It’s a collaborative effort to leverage the research strengths of Mizzou toward a better future for the health of Missourians and beyond. The Roy Blunt NextGen Precision Health building at MU anchors the overall initiative and expands collaboration between researchers, clinicians and industry partners in the state-of-the-art research facility.