Research
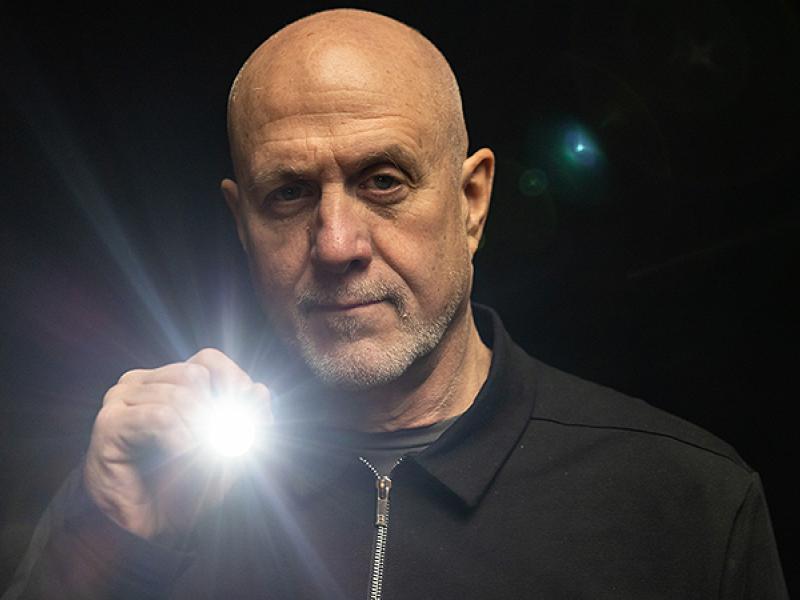
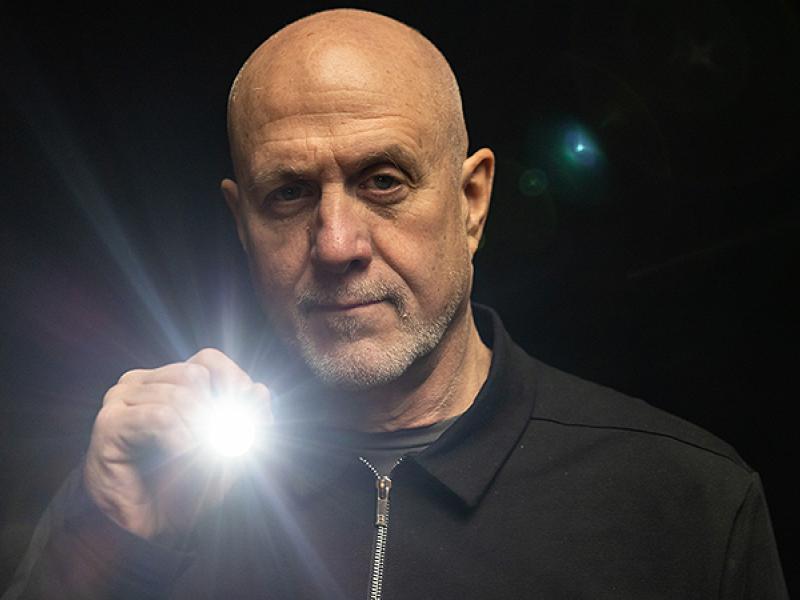
Shining a spotlight on cancer
(1/14/26) To determine who could benefit from targeted cancer treatments, a researcher at the University of Missouri is putting tumors under the spotlight.
...
This is a site-wide search. if you already know what you're looking for, try visiting a section of the site first to see A-Z listings.


MU is an equal opportunity employer.
Copyright © 2026 — The Curators of the University of Missouri. All rights reserved. DMCA and other copyright information. Privacy policy.
For website issues, contact MU Health Care Communications. Contact the MU School of Medicine.