A groundbreaking process developed by researchers based in the Roy Blunt NextGen Precision Health Building is offering new hope in the fight against blood cancers, such as lymphoma and leukemia.
A pair of researchers at the University of Missouri School of Medicine have developed a process for marking transplanted donor bone marrow cells so that the immune cells only attack cancerous cells but not healthy tissue. One of the reasons bone marrow transplants are often a last resort for patients with blood cancers is graft-versus-host disease (GVHD), a common occurrence where transplanted donor immune cells attack both malignant and healthy cells in the recipient.

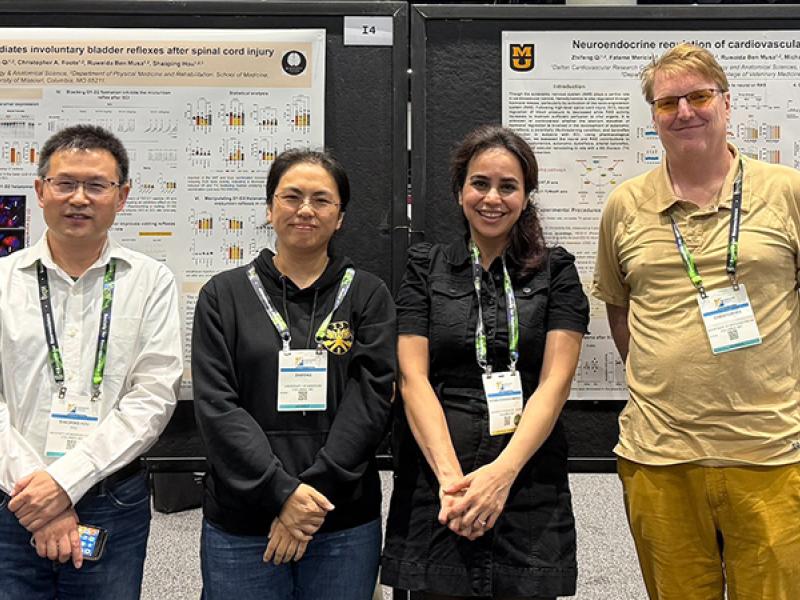
“Our ability to biologically label these donor immune cells so that they will attack cancerous cells in the host and then stop themselves from attacking healthy tissue offers new hope that bone marrow transplants can be safer and more effective for patients,” said co-lead researcher, Esma S. Yolcu, PhD, professor of Child Health and Molecular Microbiology and Immunology. “The stem cells in bone marrow have tremendous potential to combat autoimmune diseases, such as type-1 diabetes and blood cancers, such as leukemia, lymphoma and multiple myeloma. It is critical to solve the puzzle of GVHD to unlock the full potential of bone marrow cell transplant treatment regimens.”

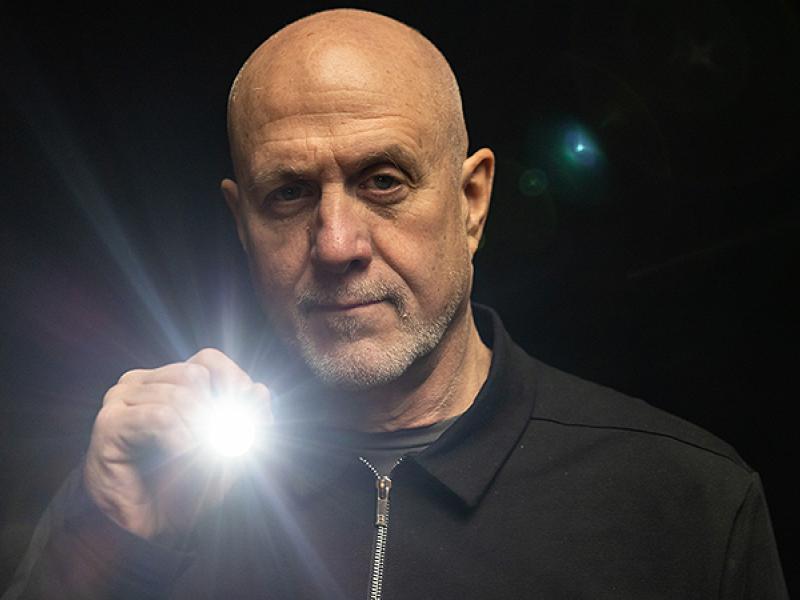
Yolcu and Haval Shirwan, PhD, also a professor of Child Health and Molecular Microbiology and Immunology and associate director of the Immunomodulation and Regenerative Medicine Program at Ellis Fischel Cancer Center, developed the ProtEx™ platform technology to generate recombinant biologics that instruct immune cells to achieve a desired treatment outcome. Engineered donor cells display on their surface instructions for the transplanted immune cells to attack only the cancerous cells and then self-destruct before attacking healthy tissue in the host, thus preventing GVHD.
“This approach has significant potential as a treatment on its own or in combination with other clinical regimens to increase the efficacy of stem cell transplants,” said Shirwan. “The process of engineering the donor cells is straightforward and efficient, making it suitable for clinical translation.”
In their research to date, the ProtEx™ engineered immune cells have been effective in overcoming GVHD following transplantation in mice as well as in a humanized mouse model. Transplantation with the engineered cells was effective in preventing acute GVHD without a detectable negative impact on the recipient immune system. The concept is presently being pursued for testing in a large animal model of GVHD as a prelude to clinical translation for the treatment of hematological cancers.
Yolcu and Shirwan’s research was recently published in Blood Advances, entitled “Engineering donor lymphocytes with Fas ligand protein effectively prevents acute graft-versus-host disease.” The lead authors disclosed that they have a provisional patent on using SA-FasL-engineered cells as a prophylactic approach for acute GVHD. The researchers also recently received a National Institutes of Health grant for their research at the Roy Blunt NextGen Precision Health Building on a treatment for type-1 diabetes that uses transplanted stem cells derived insulin producing cells to replace the need for regular insulin injections.