The vast majority of cancer survivors rely on primary care clinicians for follow-up treatments, especially in rural areas, according to a study conducted by researchers from the University of Missouri School of Medicine. Patients depend on their clinicians to help them navigate the steps in their cancer journey, often seeking their advice regarding necessary tests or to explain the oncologist’s recommendations.
The study found that roughly 96% of cancer survivors reported visiting with their primary care physician for follow-up treatment and survivorship care, with 60% of patients seeing an oncologist. The disparity is greater in rural areas, where specialized health care can be hours away and much more expensive than seeing the neighborhood doctor.
The researchers conducted interviews with 17 non-oncology, Missouri-based clinicians, with 67% practicing medicine in rural areas. They were asked about their current approach to cancer survivorship care and what they need to improve that care. The majority of those interviewed relied on training from their residency years – if they received any – and on the patient’s own oncology notes and their personal accounts of treatment.
The clinicians consistently noted that the few resources available in rural areas made treatment and outreach more difficult.

“Clinicians expressed a desire to have more access to information and online and offline trainings, like curbside consults, accessible and updated guidelines and webinars,” said co-author Mirna Becevic, PhD, an associate professor in dermatology from the School of Medicine. “More educational opportunities would be beneficial, especially to identify conditions specifically caused by cancer, or at least flag something for closer attention.”
With technology advances, the number of cancer survivors is expected to continue to rise. They are not all guaranteed access to follow-up care, however. Currently, there are about six oncologists for every 100,000 U.S. adults, with only 10% of oncologists living in rural areas. A significant hurdle to the health of rural cancer survivors.
“Cancer survivors from rural areas reported worse symptoms caused by treatment, but due to travel distance and costs, they may return to their primary care clinicians and stop seeing oncologists sooner than patients from urban areas,” Becevic said. “Patients in rural areas report feeling stressed as they face significant barriers to receive cancer survivorship care.”
The study suggests several ways to overcome these barriers, such as equipping primary care physicians with the tools they need or using technology and telehealth to expand the reach of doctors.
It’s Not Always Easy: Cancer Survivorship Care in Primary Care Settings was recently published in the Journal of Cancer Education.
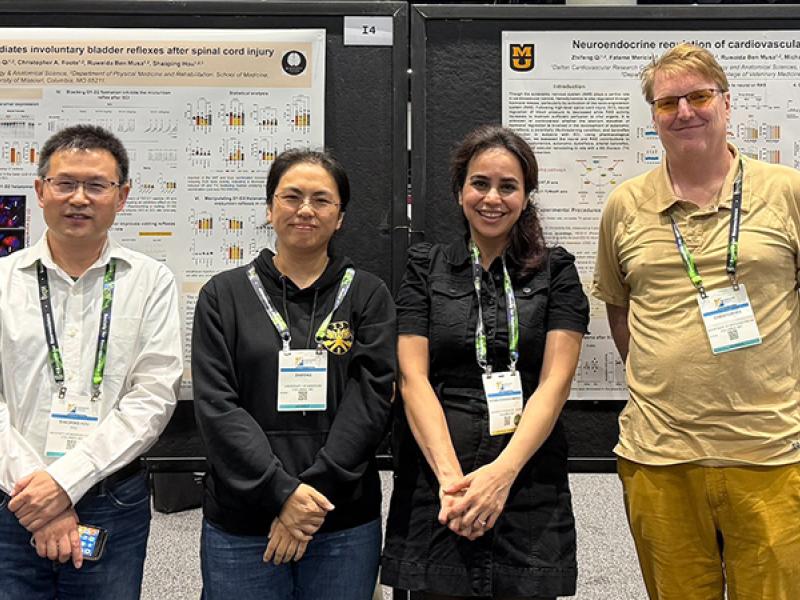
In addition to Becevic, study authors include, Allison B. Anbari, PhD, RN, assistant professor at the Sinclair School of Nursing and Jane A. McElroy, PhD, professor of family and community medicine. The authors claim no conflicts of interest.