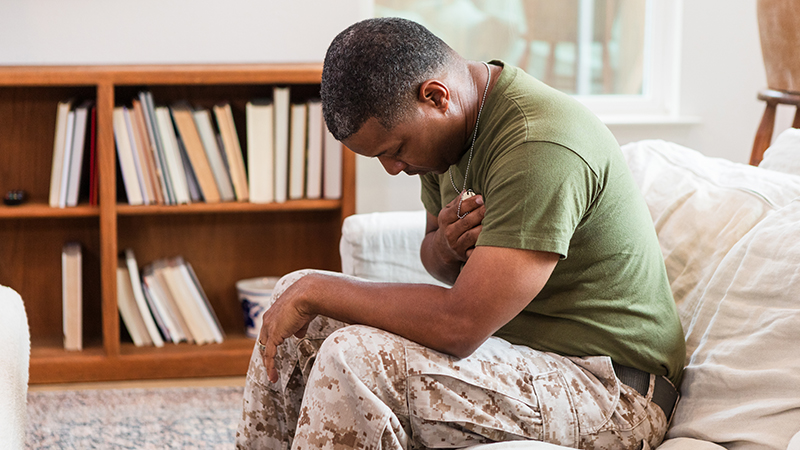
Cardiovascular disease (CVD) is the leading cause of death in the United States, with obesity strongly associated with its development. Veterans tend to have both diseases at a higher rate than non-veterans. A quartet of researchers from the University of Missouri School of Medicine and NextGen Precision Health received nearly $1.2 million through the Department of Veteran Affairs to investigate if a specific medication can help these veterans.
Based on past research, a common medication used to treat type 2 diabetes, empagliflozin – better known by the brand name Jardiance – may help with arterial stiffening, which contributes to CVD development.
“One of our long-term goals is to understand the mechanisms that cause and potentially reverse arterial stiffening,” said Jaume Padilla, co-principal investigator. “This will help identify and develop effective strategies to reduce CVD in this population.”
Arterial stiffening occurs when arteries lose flexibility, which makes it difficult for these blood vessels to contract or expand for blood flow. As a result, the heart has to work harder to pump blood and keep the flow going, causing blood pressure to rise. Currently, there are no treatments that specifically target arterial stiffening, but these researchers hope to change that.
“The era of precision medicine will allow us to tailor future treatments to the individual patient,” said Luis Martinez-Lemus, one of the collaborating investigators.
This four-year, VA-funded project will investigate how arteries become stiffer and determine if empagliflozin reduces arterial stiffness in veterans with obesity and subsequently improves their heart health.
“CVD is the silent battle many veterans continue to fight long after their service ends, and more targeted interventions are needed to address its impact,” said Camila Manrique-Acevedo, co-principal investigator.
Nai-Wei Chen, PhD is another co-investigator of this project and will serve as biostatistician. He is an assistant research professor of Biomedical Informatics, Biostatistics and Medical Epidemiology at the Mizzou School of Medicine. Camila Manrique-Acevedo, MD, is an endocrinologist at MU Health Care, the Chief of Endocrinology at the Harry S. Truman Memorial Veterans’ Hospital (VA) and a NextGen Precision Health Investigator. Luis Martinez-Lemus, DVM, PhD is a professor of Medical Pharmacology and Physiology and a NextGen Precision Health Investigator. Jaume Padilla, PhD is a professor of Nutrition and Exercise Physiology, a NextGen Precision Health Investigator and a research health scientist at the Truman VA.

Highlighting the promise of personalized health care and the impact of large-scale interdisciplinary collaboration, the NextGen Precision Health initiative is bringing together innovators from across the University of Missouri and the UM System’s three other research universities in pursuit of life-changing precision health advancements. It’s a collaborative effort to leverage the research strengths of Mizzou toward a better future for the health of Missourians and beyond. The Roy Blunt NextGen Precision Health building at MU anchors the overall initiative and expands collaboration between researchers, clinicians and industry partners in the state-of-the-art research facility.