Research is a major component of the Department of Ophthalmology and it encompasses both the basic and clinical sciences. Research laboratories and support facilities span the entire second floor of the Mason Eye Clinic with additional space located across the street at the Harry S. Truman Memorial Veterans' Hospital as well as space at the MU Veterinary Medical Diagnostic Lab and the MU School of Medicine Lab.
Our multidisciplinary approach leads to advances in medical science and clinical treatments. Research interests within the department are diverse and cover a wide range of ophthalmologic problems.
Basic Science Research
The Neurodegenerative Diseases Research Laboratory (NDRL) is dedicated to discovering the causes of and developing treatments for diseases that involve degenerative changes of the nervous system, including the retina, brain, spinal cord, and peripheral nerves. The laboratory is directed by Martin Katz, PhD, and focuses on determining the mechanisms underlying age-related retinal degeneration, a leading cause of blindness in the United States.
The research and lab of Rebecca Whiting, PhD, focus on developing therapies for inherited retinal degenerative and neurodegenerative diseases. Her team studies the CLN2 form of Batten disease in a naturally occurring canine model and is investigating AAV gene therapy in addition to a stem cell-based therapy for this disease. The lab also works to identify additional biochemical, behavioral, and imaging-based biomarkers that can be translated for use in children with CLN2 disease to better monitor disease progression and evaluate efficacy of therapy.
Rick Fraunfelder, MD, and Xu Han, MD were recently awarded a $25,000 Coulter Grant to support their research on corneal tissue cryopreservation.
Normal visual function of the eye requires retinal homeostasis maintained by the blood-retinal barrier (BRB), which is impaired in various retinal diseases, including diabetic retinopathy (DR) and age-related macular degeneration (AMD). Dr. Hu Huang’s primary research interest is to decipher the molecular and cellular mechanisms that underlie BRB integrity and impairment in retinal health and disease. Vascular endothelial cells and retinal pigment epithelium (RPE) are the fundamental cells of the inner (i) and outer (o) BRB, respectively. Other retinal cell types, such as pericytes, neurons, and glia, reinforce BRB structure and function. One of Dr. Huang’s projects elaborates on the role of placental growth factor (PlGF) in regulating iBRB function both in vivo and in vitro. Another project explores the role of CXCR5 GPCR signaling in RPE homeostasis and oBRB function. The evidence indicates that CXCR5 signaling is involved in AMD. Dr. Huang’s third project is to vet retinal cell communications mediated by exosomes. Overall, Dr. Huang’s research is devoted to understanding the pathophysiology of retinal diseases and identifying therapeutic targets for DR and AMD treatment.
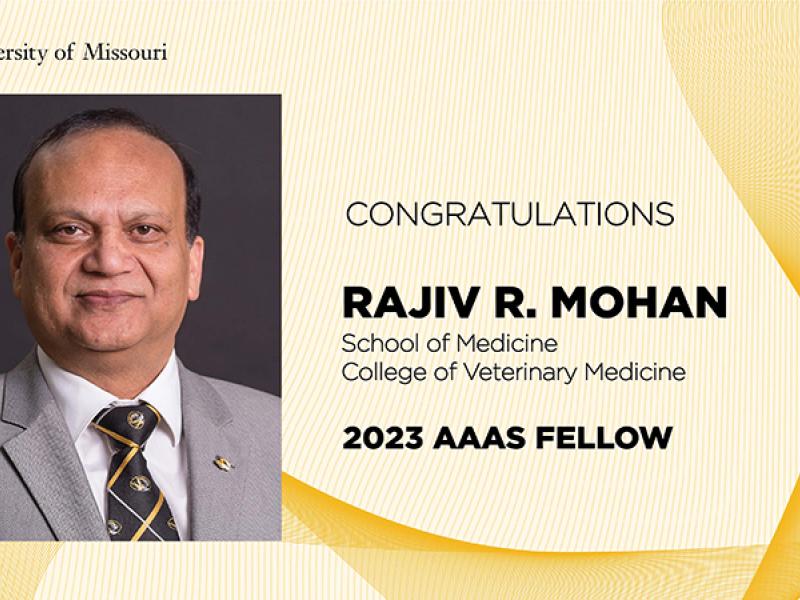
The cornea is an ideal candidate for gene therapy due to its immune-privilege status, accessibility and easy visual monitoring. Corneal haze, scarring and neovascularization are among the leading causes of vision impairment in the world and affect approximately 1.5 million Americans every year. Abnormal wound healing due to corneal injury or infection has been shown to play a critical role in causing these and other corneal disorders and diseases. The research in the laboratory of Rajiv Mohan, PhD, is primarily focused one developing tissue-targeted selective gene therapy approaches for preventing/treating corneal disorders, diseases and dystrophies, and studying the cellular and molecular mechanisms involved in corneal wound healing.
The studies underway in the Krishna Sharma, PhD laboratory are not only unraveling the molecular mechanisms of age-related lens crystallin modifications and aggregation but also aimed at identifying potential strategies for inhibiting aggregation of crystallins and lens opacification. Specifically, he is studying the structure–function of lens crystallins, the process of lens protein aggregation, the interactions of crystallin subunits and how they are affected by mutations or age-related modifications. Understanding the molecular mechanisms involved in keeping the eye lens transparent or turning it to opaque tissue will enable researchers to design treatment modalities to delay cataract formation. In addition, he is also involved in the synthesis and characterization of peptides that have chaperone-like activity with an intent to advance them to become therapeutic molecules for human diseases arising from protein aggregation such as Alzheimer’s and Parkinson’s diseases, Amyotrophic lateral sclerosis, dementia with Lewy bodies, Huntington’s disease etc.
Protein misfolding and aggregation is the primary cause of many diseases including Alzheimer's disease, Parkinson's disease, cataract, diabetic retinopathy, certain corneal dystrophies, Glaucoma, type 2 diabetes, amyotrophic lateral sclerosis (ALS) and cystic fibrosis. Prevention of protein misfolding associated proteinopathies and maintaining cellular homeostasis is crucial for controlling these diseases. Santhoshkumar Puttur, PhD, is involved in designing and testing peptide chaperones that are cell-permeant and protease-resistant to contain protein misfolding conditions and increase longevity. He is developing chaperone peptides that show on-demand action and preparing mini-gene constructs that would open new avenues for treating protein conformational diseases.
Dry eye disease (DED) is a common complaint as it affects one in five people, and the number is expected to increase as people age. In mild cases, signs and symptoms may include a stinging, burning or scratchy sensation in your eyes. Moderate to severe DED is often associated with significant pain, poor vision clarity, and reduced quality of life and productivity. The existing therapies for DED are merely palliative and often provide inadequate relief of symptoms. The focus of the DED research program, directed by Lixing W. Reneker, PhD, is to understand how age-related factors, such as decline or deficiency of growth factors and sex hormones, affect the functions of tear-production glands. Our goal is to develop targeted therapies to prevent and treat tear gland dysfunction and to improve the quality of life in the aging population.
Clinical Research
Dean Hainsworth, MD is involved in several research projects. The AREDS 2 trial is an NIH sponsored clinical trial to determine whether Lutein/Zeaxanthin or Fish Oil would further decreased the risk of choroidal neovascularization in patients with AMD. The DCCT/EDIC is a long term NIH sponsored trial following patients with type 1 diabetes to further determine benefits of careful glucose control including examining the development of retinopathy. The DEGAS is a Pfizer sponsored trial to determine whether injecting a study drug (siRNA to inhibit expression of hypoxia inducible gene) improves diabetic macular edema. Dr. Hainsworth is also exploring the use of gold nanoparticles as a platform to deliver anti-angiogenic drugs to specific targets in the eye as a potential treatment for ocular neovascularization.