Pre-clinical research uses cells (in vitro) and animals (in vivo) to better understand disease biology and develop potential treatments. This process must occur before a new treatment is tried in people to ensure that it is safe and has the best chance of being effective.
Because humans are so complex, one of the major challenges of pre-clinical research is the availability of models that accurately reproduce the disease state being studied. Good pre-clinical models are essential for successful translation to humans.
Within the Department of Physical Medicine and Rehabilitation, our scientists apply cutting-edge neuroscience techniques along with clinically relevant measurements of physical and mental function to explore the effects of different treatments on models of Spinal Muscular Atrophy, Charcot Marie Tooth Disease, aging, Alzheimer’s disease, Spinal Cord Injury, and Amyotrophic Lateral Sclerosis to name a few. Please click on the links for the labs below to learn more about their ongoing work.
Arnold Lab
Dr. Arnold’s research program is focused on translational neuromuscular physiology in the context of health, aging and disease. His lab leverages clinical and preclinical studies to understand mechanisms of biological aging of the nervous system as well as genetic, acquired and sporadic disorders of muscle and the motoneuron. Adding years to a person’s life is not Dr. Arnold’s primary goal. Instead, he is interested in mechanisms of decline of the nervous system and muscle during aging and understanding ways to improve resiliency of nervous system function across the lifespan.
Castoro Lab
Dr. Castoro leads a translational neuroscience lab which focuses on understanding the genetic, as well as epigenetic determinants of peripheral nerve disease and how these can be reversed. As part of their approach, they are developing quantitative ultrasound as a biomarker to measure axonal degeneration in humans and in murine models. In addition, they utilize murine and direct induced motor/sensory neuron models to elucidate DNA methylation regulated neuronal degeneration of the peripheral nervous system.
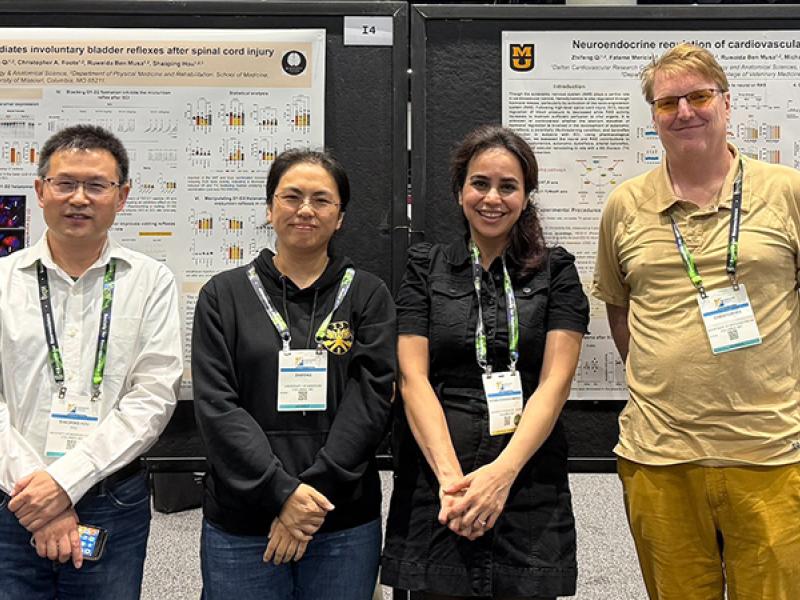
Hou Lab
The research work of Shaoping Hou, PhD, focuses on autonomic dysfunction following traumatic spinal cord injury (SCI), specifically lower urinary tract and cardiovascular dysfunctions. Dr. Hou employs multidisciplinary approaches, including neuroanatomical, physiological, genetic, and cellular and molecular techniques, to elucidate supraspinal and intraspinal neuronal machinery of these disorders. Utilizing a variety of strategies, such as neural progenitor cell transplantation, axon regeneration, passive exercise, and cell reprogramming, his team attempts to rebuild neuronal pathways for autonomic functional recovery.
Moss Lab
Dr. Moss’s research is focused on identifying cellular and molecular mechanisms driving Charcot-Marie-Tooth disease (CMT) pathogenesis. CMT is one of the most common inherited neurological disorders, yet there are no treatments currently available to patients. Dr. Moss is using advanced mouse and cellular models to dissect CMT pathomechanisms and systems neuroscience to study CMT pathophysiology. Her work aims to identify novel therapeutic targets and strategies for CMT.
Saxena Lab
Dr. Saxena’s main research aim is to identify cellular mechanisms causally involved with the onset and spreading of neurodegenerative diseases. In her work, she uses cutting-edge imaging and human cellular models combined with systems biology to identify and investigate disease-related aberrant cellular mechanisms, which form the framework for future novel therapies.