The goal of rotating in the cardiac intensive care unit is to train fellows in the care of acute, life-threatening cardiovascular conditions, including but not limited to: acute coronary syndromes and associated mechanical complications, acutely decompensated heart failure with and without mechanical circulatory support, circulatory collapse/shock, complex ventricular arrhythmias, unstable conduction disturbances, pericardial tamponade, aortic dissection, hypertensive emergency, massive pulmonary embolism, and severe pulmonary hypertension.
Fellows will be able to integrate clinical, electrocardiographic, hemodynamic, and imaging data to manage acutely ill patients. Fellows will be expected to take a leading role in the care of patients and house staff education, as well as interact professionally with patients, families, and all members of the care team.
Rotation leaders
- Dr. Arun Kumar (MUHC)
- Dr. Poorna Karuparthi (VA)
Objectives
1st rotation
- Recognize differential diagnosis of shock and hemodynamic characteristics of each type.
- Interpret hemodynamic data and apply to the management of the patient.
- Understand indications, contraindications, and mechanism of action of vasoactive, inotropic, anticoagulant, antiplatelet, and fibrinolytic medications.
- Manage patients with acute coronary syndromes including associated rhythm disturbances and mechanical complications of acute myocardial infarction, initially with supervision.
- Diagnose and treat hypertensive emergency.
- Diagnose and manage acutely decompensated heart failure, understanding indications for inotropic therapies and mechanical circulatory support, initially with supervision.
- Review types of mechanical circulatory support and their indications/contraindications.
- Diagnose and manage acute, severe valvular heart disease, initially with supervision.
- Diagnose and treat unstable arrhythmias with medications and/or defibrillation, initially with supervision.
- Diagnose pericardial tamponade and recognize indications for pericardiocentesis.
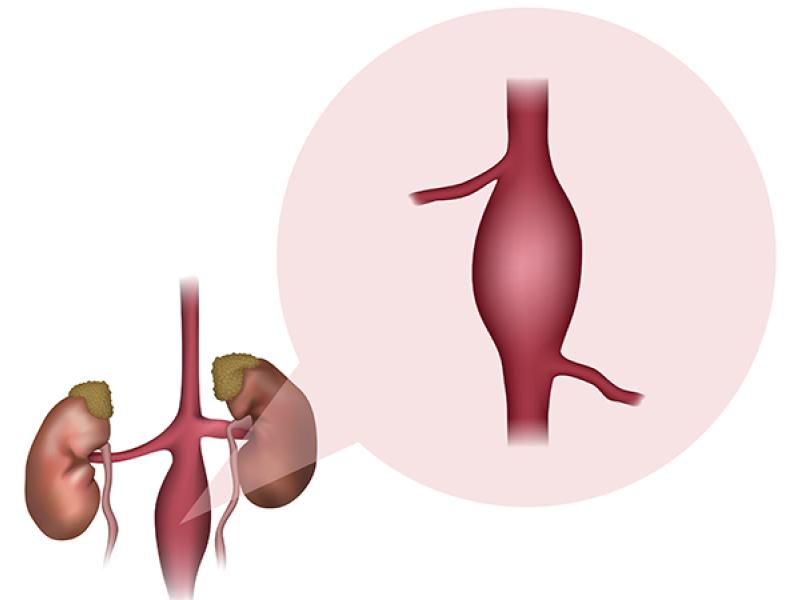
- Review indications for surgery in aortic dissection.
- Recognize indications for oxygen supplementation, endotracheal intubation, and mechanical ventilation.
- Review indications for hemodialysis.
- Apply hypothermia protocols for patients with cardiac arrest.
- Perform central venous catheter insertion, arterial catheter insertion, and emergency echocardiography independently.
- Perform pulmonary artery catheter insertion and temporary transvenous pacemaker implantation under supervision.
- Manage spontaneous or treatment-related acute bleeding complications.
- Participate in family meetings, integrate palliative care, and assist in discussions regarding end-of-life care and transition to hospice.
2nd and 3rd rotations
In addition to the above:
- Review risk stratification scoring systems for acute coronary syndrome, acutely decompensated heart failure, and pulmonary hypertension.
- Evaluate and manage severe pulmonary hypertension, including indications, contraindications, and mechanism of action of pharmacologic therapies.
- Recognize indications for urgent/emergent valve intervention in patients with severe valvular heart disease.
- Diagnose complications of transcatheter valve interventions and determine appropriate interventions for management.
- Manage postoperative cardiac patients and recognize postoperative complications as part of a management team.
- Diagnose and manage hemodynamic instability after cardiac surgery.
- Participate in peri-operative care of cardiac transplant and left ventricular assist device recipients as a part of the management team.
- Review treatment of hypotension in specific populations such as cardiogenic shock, hypertrophic obstructive cardiomyopathy, right ventricular infarction, massive pulmonary embolism, severe pulmonary hypertension, pericardial tamponade, and distributive shock.
- Perform pulmonary artery catheter insertion and temporary transvenous pacemaker implantation independently.
- Perform pericardiocentesis in emergency settings.
- Manage hemodynamic support devices and manage large bore vascular access
- Lead the CCU team of residents and other learners, with appropriate faculty supervision.
Description of teams
At MU Health Care, the CICU team is composed of two residents, one cardiology fellow and one cardiology attending physician. At the Harry S. Truman Memorial Veterans’ Hospital, this service is usually composed of a cardiology attending physician, a cardiology fellow, and a medicine resident (the latter individual also has a role with the MICU team). They are directly responsible for patients admitted to the VA CICU. the fellow and attending also provide consultative service for patients admitted elsewhere in the VA hospital. The night float fellow covers all the above services as well as cardiology consultation requests between 6 p.m. and 7 a.m. In addition, the MUHC CICU fellow and the night float fellow provide backup to the inpatient cardiology team at University Hospital that includes a cardiology attending and residents when needed.
Fellow responsibilities
- Round on CICU patient with the team, be familiar with all patients’ plan of care and participate in making decisions.
- Evaluate all new patients admitted to CICU from 7 a.m. to 6 p.m.
- Evaluate new patients admitted to Cardiology ward team and CICU while on night float
- Discuss the above-mentioned admissions with the resident and medical student on service, to develop an appropriate differential diagnosis, proposed work-up plan, and initiate therapy.
- Conduct daily ‘work’ rounds with residents, students, nursing and other health care personnel in CICU, to include ethical, cost-containment, social issues as well as medical and discharge planning issues, and triage for transfer out of CICU at the earliest time each morning.
- Expected to help with carrying CICU patients if total CICU patient load is more than residents cap especially if one of the residents is off.
- Respond to code STEMI in non-cardiology inpatient services.
- Provide backup for emergency consults when cardiology consult fellow is in clinic.
- Provide teaching for residents and students.
- Provide appropriate supervision of residents and students in procedures such as insertion of central lines, PA catheters, temporary pacemakers, arterial lines, and thoracentesis and pericardiocentesis. Preferably, these will be done with the CICU attending present as well.
- Manage hemodynamic support devices and large bore access with attending supervision.
- Provide appropriate triage support for the residents in deciding transfers to and out of CICU, as well as discharge planning, including discharge medications.
- Ensure efficient patient flow.
- Maintain effective, day-by-day communication with CICU patients, their families, and with nursing personnel, with respect to medical care, diagnosis, medical testing, and prognosis, especially with critically ill patients.
- Communicate with referring physicians at the time of referral, significant in-hospital events, and at discharge.
- Provide basic and advanced cardiac life support for cardiology patients.
- Evaluate admissions in the ER with attention to triage for appropriate placement in CICU, step-down, or telemetry.
- Review chest X-rays, ECG’s, telemetry rhythm strips, coronary angiograms, echocardiograms, myocardial perfusion scans, and stress tests on all new admissions to CICU and for night float coverage of any patient.
- Maintain the highest level of professionalism, ethics, and of medical care for each patient without regard for social, religious, ethnic, or gender differences.
- Wash hands before and after each patient contact.
- Ensure communication with any physicians consulted, with expressed appreciation and due regard for recommendations given, in the best interest of the patient.
- Maintain open communication with the CICU attending, who will be available for daily attending rounds, procedures, and at other times deemed necessary for good patient care.
- Daily review of resident progress notes for accuracy in documentation of the ongoing plans and reassessment as new information becomes available.
- Enroll patients in research projects.
- Present patient information at M&M conference or other conferences.
Attending responsibilities
The faculty attending is directly responsible for all patient care. The attending is available for procedures requiring direct supervision. The attending is responsible for teaching, both formally and informally, during the rotation.