In 2023, we began planning a change to our formal didactic program. The system we had was a one-hour conference each weekday, mid-day, with a rotating series of topics. We wanted to improve engagement, effectiveness, and satisfaction. We consulted with national leaders in neurology education. We researched adult learning theory and best practices in medical education. We built a new didactic curriculum centering on a weekly ½-day session for one afternoon each week rather than daily brief conferences.
For our new system, the neurology department rearranged faculty schedules, cancelled Wednesday afternoon clinics, changed time for the weekly grand rounds, changed schedules for faculty meetings and faculty mentoring sessions. We worked with the department to manage clinical coverage of inpatient services while residents leave for the entire afternoon every Wednesday.
Our new system uses a variety of learning tools. We draw from a library of video lecture material. We use local resources, including our institution's medical education simulation lab, to create weekly hands-on activities. Our curriculum addresses how to study, how to take tests, and how to prepare for taking boards. Our curriculum addresses every specific topic mandated by the ACGME, including multiple-choice boards-type questions each week to assess resident competency in all such areas. We thus ensure that on a 3-year recurring cycle, didactic content and competency assessment includes coverage of behavioral neurology, child neurology, clinical neurophysiology, epilepsy, headache, infectious disease, movement disorders, neurocritical care, general neurology, neurogenetics, neuroimaging, neuroimmunology, neurology of aging, neuromuscular medicine, neuro-oncology, neurotology, neuro-ophthalmology, neuropathology, pain management, sleep disorders, vascular neurology, and topics of professionalism.
Our new system went live July 1, 2024, and we are executing it even as we continue to build it. We will survey residents and faculty in a process of continuous quality improvement, as we continue to grow and develop our didactic offering.
Program Components
- Grand Rounds: 12pm - 1pm. All residents attend, marking the end of their clinical or other work activity for the day.
- Core Topic Video: Residents watch assigned video lectures. The assigned videos fit into a “core” theme for the day, rotating every week: vascular, movement, epilepsy, neuromuscular, cognitive/behavioral, headache, neuroimmunology, professionalism. Assigned videos can be as brief as 20 minutes, and can be different for PGY2, PGY3, or PGY4 residents. Thus, over a 3-year cycle, we can cover a wide range and graduated levels of content. Residents have access to the video library on their own time, too.
- Core Hands-on Activity:Keeping with the day’s “core” theme, residents do a hands-on interactive activity relevant to that core topic. Example hands-on activities could include simulated proctored encounters with standardized patients, botulinum toxin injection training, performing neurocognitive testing, practice doing electromyography or nerve conduction studies, Neuro Jeopardy!, reading EEGs, case discussions, demonstration of specific neurologic exam techniques, and programming deep brain stimulation.
- Non-Core Lecture: These are usually live lectures covering content not captured by the 8 recurring core topics. Once a month this session includes meeting with a neuropathologist to view neuropathology slides, and once a month this session includes meeting with a neuroradiologist to view neuroimaging. Non-core lectures help ensure that over a 3-year cycle, we have didactic mechanisms to cover all needed neurology curricular content.
- Localization Exercise: This is a faculty-driven interactive case discussion, often led by the residency program director. It begins with random selection of a patient from last week’s resident continuity clinic. All view the resident’s note for the encounter. The resident describes and defends possible locations of neurologic dysfunction for the presenting complaint. The resident answers questions. Other residents are also called on to discuss how to localize neurologic dysfunction. Discussion includes best practices in getting a neurology story, writing a note, and other topics in clinical neurology practice.
- "STP" (Studying, Test Taking, Preparing for Boards): Weekly instruction focusing on a new tip each week. The focus is on data-driven, emphasizing adult learning theory and other lessons from cognitive psychology.
- Multiple-Choice Question Assessment: Each resident uses their own device to answer 10 boards-style multiple choice questions, each resident answers questions on their own. After all residents submit their individual responses, the group discusses the one item that was missed by the greatest number of residents, focusing on test taking strategies. Over a block of 8 weeks, the questions change but they all focus on a single specific recent issue of the journal Continuum. The department purchases a subscription for each resident. Continuum is a well-refereed publication from the American Academy of Neurology. Over a 3-year cycle it covers all the topics that the American Board of Psychiatry and Neurology lists as the topics covered by the boards exam in adult neurology. To demonstrate competency, over the 8 weeks that the Continuum issue is being tested, each resident must at least once answer 8 out of 10 questions for a 10-item test.
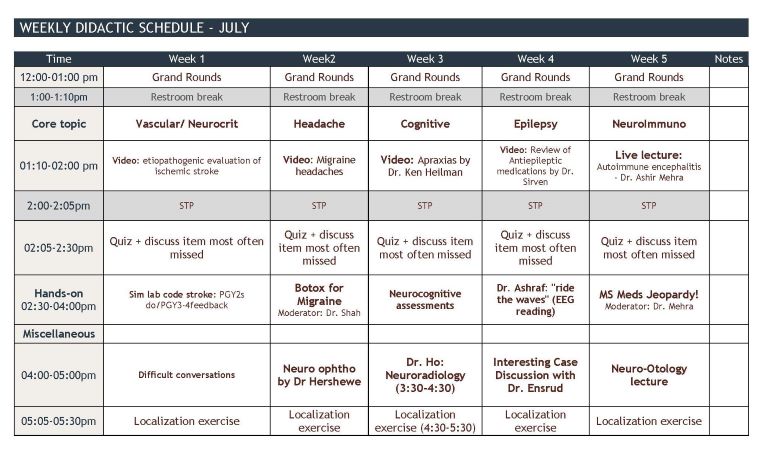
Below is a sample schedule for a month.